Skin stem cells reduce their renewal rate in response to cancer-driving mutations
Former graduate student Cai, a postdoctoral medical scientist in training, took on the challenge. She focused on learning how skin tissue handles widespread mutations in a gene called H-Ras, which is mutated in Costello syndrome, an inherited disorder that affects many systems of the body and increases cancer risk.
The Ras gene family controls cell growth. Many human tumors contain mutations that spur cell growth by making a Ras family member permanently active. One study found that having a RASopathy raised the risk of childhood cancer by 10-fold. (On average, the risk of developing cancer in childhood is 0.33%, or 1 in 300.)
Cai chose to examine the effect of permanently activating H-Ras in every cell of the body, mimicking inherited mutations found in people with Costello syndrome. She genetically modified mice so that all the cells in their skin turned on a mutated form of H-Ras, which is associated with cancer in humans.
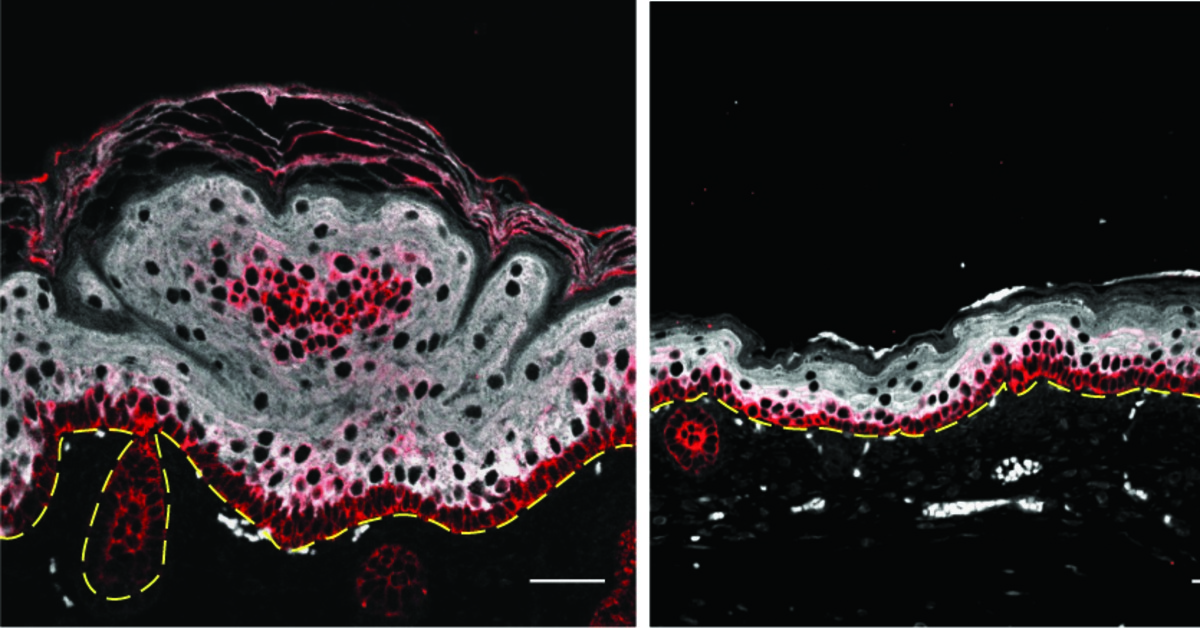
Cai found that though there were signs of skin cell overgrowth, or proliferation, in mutant mice, the animals did not form tumors, and the excess growth was less than she and her colleagues had expected. After ruling out other ways the cells might have reined in their growth, she measured the stem cell renewal rate. Cai found that stem cells with active H-Ras had significantly turned down their renewal rate, suggesting that they had shifted to producing more skin cells but replacing stem cells less often.
“This increase in proliferation seems to be balanced by reduced renewal, but still renewal that ensures long-term maintenance [of the skin tissue],” Beronja said. “So it's a qualitatively different result that basically ensures that tissues in these people don't collapse and are actually maintained.”
Protein production fine tunes stem cell renewal
Cai next wanted to determine the cellular process skin stem cells use to ramp down their renewal rate. Work from other scientists gave her a clue. Other labs had shown that a cellular process called translation was linked to renewal and proliferation: more translation correlated with increased cell growth and division and reduced renewal.
Translation is a key step in the system our cells use to make the information encoded in our genes tangible. Our DNA encodes the proteins that make all of our cellular processes possible, but it takes a few steps to get from DNA to protein. First cells copy the information in DNA into a new form, creating molecules called messenger RNA, or mRNA, which cellular protein-making factories use as the instruction for building proteins. They read, or translate, these mRNAs into proteins. Cells can fine tune how much genes are turned on by changing how and when translation occurs.
Cai measured the translation rate in skin stem cells to see if it changed in response to the presence of mutated Ras. She found that the translation rate in skin stem cells from mutant mice was higher than in skin stem cells in normal mice. Reducing H-Ras activity also reduced the translation rate in mutant skin stem cells.
She screened genes known to be involved in translation to see if any influenced skin stem cells’ proliferation or renewal rate when H-Ras was permanently active. Out of the 200 genes whose effects Cai examined, one stood out: eif2b5. This gene is part of the molecular complex that initiates the translation of mRNA to protein. When Cai suppressed mutant cells’ ability to make eif2b5 protein, their translation rate dropped. This didn’t change the translation rate in normal cells.
Cai found that eif2b5 also appeared to be causing the increased growth and decreased renewal seen in H-Ras-mutant skin stem cells. When she genetically manipulated mice with mutant H-Ras to reduce eif2b5 levels in their skin stem cells, this reduced proliferation and increased renewal. Again, changing eif2b5 levels in healthy mice did not affect the renewal rate or growth rate of their skin stem cells.
“We were totally surprised,” Beronja said, “Because again, when you think translation, you think a general process — this suggests that there's some specificity.”
And, he noted, “If you knock down eif2b5, it reverts, basically, to wild-type tissue. [The knockdown] completely fixes it, and there’s no effect in the wild-type background.”
Cell’s protein-recycling system involved in control of stem cell renewal
Working with Hutch translation expert Dr. Andrew Hsieh, Cai discovered that overactive H-Ras only ramped up translation of a subset of mRNAs. About 40% of these were specifically controlled by eif2b5. Together with members of the Hsieh Lab, they found that these mRNAs have a characteristic sequence that attracts molecular complexes containing eif2b5, ensuring specific, rather than general, control.
Surprisingly, Cai found that in skin stem cells with overactive H-Ras, eif2b5 reduced the cells’ ability to self-renew by increasing translation of genes that direct proteins to the cells’ protein-recycling system, in which proteins are degraded and their components reused.
She and Beronja had expected that skin stem cells would regulate their “stemness” by changing the levels of proteins whose job it is to turn genes on. But turning genes on takes time. By drawing on the protein-recycling system, skin stem cells may be able to quickly remove renewal-promoting proteins from circulation.
When Cai blocked this process in mice with mutated H-Ras, she found that they formed skin tumors more quickly than mice whose skin stem cells were allowed to handle mutated H-Ras normally. After about 30 days, half the mice with mutated H-Ras and reduced cellular protein recycling had developed tumors; it took nearly 50 days for half the mice with only mutated H-Ras to develop tumors. In contrast, enhancing protein recycling in mice with mutated H-Ras further extended the time they lived without developing tumors.
Understanding the system
Beronja’s main concern now is to uncover the mechanism by which the protein-recycling system controls skin stem cell renewal. Presumably the cells are using the system to break down specific stem cell factors, but they remain to be discovered.
Beronja also thinks that the findings could help explain more about how cancer develops generally. Age is one of the biggest risk factors for cancer; this is generally attributed to the fact that as we age, we accumulate more mutations. But perhaps this self-correcting ability to “tolerate” oncogenic mutations fades with time?
“It's quite possible that ability to handle [cancer-driving mutations] eventually goes away. And it could be one of the explanations of why cancer is a disease of older people,” he said.
Beronja didn’t expect to find that translation could slow tumor growth. The conventional scientific wisdom has been that translation usually helps drive cancer: Tumor cells need proteins to grow, and to make proteins they need to increase production.
“In this case, we actually showed that increased translation is tumor-suppressive,” Beronja said.
This highlights a potential drawback to therapeutic strategies that aim to halt tumor growth by restricting translation, he said. As drugs to inhibit translation are increasingly being explored as anti-cancer agents, Beronja hopes scientists bear in mind that broad changes in translation could have unintended, and possibly negative, consequences for cancer growth.
“I think it’s a cautionary tale,” he said. “Basically, don’t target something you don’t understand.”
The National Institute of Arthritis and Muskuloskeletal and Skin Diseases and the National Cancer Institute funded this work.
"correct" - Google News
June 13, 2020 at 01:22AM
https://ift.tt/2YrSjHf
Mutated skin stem cells self-correct to prevent cancer - Fred Hutch News Service
"correct" - Google News
https://ift.tt/3d10rUK
https://ift.tt/35qAk7d
Bagikan Berita Ini














0 Response to "Mutated skin stem cells self-correct to prevent cancer - Fred Hutch News Service"
Post a Comment